
Grand Discount – Buy 1, Get 1 for Free
The death of a child is the greatest reason to doubt the existence of God.
F. Dostoyevsky
“Patient incoming!!!” The triage nurse screams entering the trauma bay. You were daydreaming about a barbecue and almost forgot you’re on call this September weekend with a pregnant lady coming after a motor vehicle accident.
Around you, the most basic trauma team: 2 nurses, one ObsGyn colleague, an anesthetist on his way, and you (as narrators we still have to figure out if you are lucky or someone put a jinx on you).
The prehospital team starts the hand-over:
A – 35 yo woman, pregnant at 36 weeks;
T – 45 min ago;
M – Car accident, T-bone mechanism on passenger’s side, pt driver with the belt on, airbag exploded;
I – Short loss of consciousness, pain in the left chest, belt sign on the belly, right leg fractured;
S – 100/50 mmHg, 143 bpm R, Sat 96% on room air, GCS 13 (E3,V4,M6);
T – 2 IV lines, 250 cc of NS, Fentanest 50 mcg, C-collar & spine board.
Introduction
According to the literature, trauma may complicate up to 7-8% of pregnancies (in USA series), being the first non-obstetric cause of death for the fetus and carrying maternal mortality of 20-46%.
The causes of death in this particular population are not different from those of the general trauma one: hemorrhagic shock and traumatic brain injuries.
Approximately 50% of the mechanisms are from motor vehicle accidents, 25% from falls and the remaining are assaults, penetrating injuries, and burns.
Activating a Trauma Code
Usually, it is quite useful to remember the ATLS criteria for a trauma team activation (reported in the following table). However, the code should be also activated if, during a minor trauma mechanism, one or more of Buchsbaum’s criteria are found: hematuria, loss of consciousness and/or open fracture.
| Physiologic | Anatomic | Trauma Mechanism |
|---|---|---|
| GCS <13 SBP <90 mmHg RR <10 or >29 No peripheral pulses | Penetrating trauma Unstable thorax Burn >10% BSA Fx >2 long bones Paralysis >1 limb | Fall >4 m Speed >70 km/h Ejection Vehicle deformation Extraction >20 minutes Death on the scene |
Initial Management
The fact that you have to treat two patients at one time shouldn’t scare you, remember that the fetus is strictly connected to the mother, so, first thing, call for an obstetrician who could care for the baby, leaving you to focus only on the mother!
Caring for the mother is the only way to care for the baby!
The obstetrician should start fetal monitoring as soon as possible for pregnancies longer than 23 weeks. So you don’t have to!
The primary evaluation of the patients must be done following the ABCDE approach (according to ATLS and ETC protocols).
But how does each letter change due to pregnancy?
A – Airway:
During pregnancy, diffuse soft tissue edema will develop including at the pharyngeal/laryngeal level (increased Mallampati and Cormack score). Moreover, we need to remember that gastric emptying is slowed so always consider this kind of patient at risk for vomiting and aspiration!
If intubation is needed, do it with a rapid sequence protocol, using a video-laryngoscope (if you can), and put in an orogastric tube as soon as the airway is controlled.
B – Breathing:
A pregnant woman has increased O2 consumption by approximately 20%, so SatO2 below 95% should be avoided.
In the case of intercostal drainage, remember that the diaphragm is pushed cranially, so you should search for the fourth or third intercostal space (or, if you have the possibility and time, you may help yourself with ultrasound).
Lastly, during the last trimester of pregnancy, women have a physiologic hypocapnia due to tachypnea (the diaphragm is pushed cranially). Therefore, if you have an ABG with a PaCO2 of 35-40 mmHg, this means the woman is close to respiratory failure! Do not underestimate this!
C – Circulation:
Physiologically speaking, a pregnant woman prepares herself for a possible massive hemorrhage during labor. This means her total circulating volume of blood (especially the “plasma” part) increases. Trauma-speaking, this will hide the “normal” expected response to hemorrhages, such as tachycardia and hypotension, that would appear to appear only after a 20% loss of volume. In other words, do not wait until tachycardia comes in to resuscitate a woman, because when it comes you may be already too late with your treatment!
The uterus, after 20 weeks of pregnancy, may push on the inferior vena cava (IVC) when the woman is laying flat, thus reducing the heart preload and giving her hypotension. It is always a great idea to displace the uterus to the left side of the patient, away from the IVC, lying on the right side of the abdomen. This maneuver can be done manually or by putting a pillow below the spinal board to have a 15-30° left inclination while maintaining the inline spinal immobilization.
The use of vasopressors should be done cautiously, they will reduce the uterine blood flow! Also, the correction of metabolic acidosis with bicarbonates may decrease compensatory hyperventilation and fetal oxygenation. Both things should be avoided in a trauma case… If you are starting inotrope infusion on a trauma case, are you sure you are not wasting time to stop the bleeding? And the same question applies to metabolic acidosis! The first reason for both is ongoing bleeding!!!
This is basic, but remember: if you have an unstable patient with positive E-FAST, the treatment is in the OR!
If you need transfusions, it is always better to use a 0 negative blood! Even better if you have the time to cross-match the blood.
One more thing, during pregnancy, fibrinogen levels will rise two times (2.5-6 g/L). If you find normal non-pregnant values on blood tests, the patient may be coagulopathic as for DIC.
D – Disabilities:
The D letter does not change so much. We will have to evaluate GCS, pupils, and lateralizing signs. The only thing we will have to do is maintain the left lateral tilt of 15-30°.
What we have to pay attention to is the possible neurological alteration due to proper obstetric pathologies such as eclampsia, but remember that you need to rule out any possible trauma-related causes of altered GCS first.
E – Exposition:
Hypothermia is extremely risky for pregnant women, as we know it is strictly correlated to coagulopathy, and we are speaking of a patient where the thrombotic state is already elevated (higher fibrinogen level and increased coagulation factors).
In case of domestic violence, do not forget to check the posterior part of the patient (look at every inch of the patient’s skin).
F – Fetal:
Yes, we said we may only have to care for the mother, but the baby is there, so few things we need to bear in mind.
As we said earlier, is it fundamental to have an obstetrician at your side as soon as possible: a correct US evaluation and proper monitoring of the baby’s heartbeat are extremely important.
In case of possible premature labor, to speed up the fetus’ pulmonary development, it is possible to administer steroids (i.e. betamethasone) to the mother, according to hospital protocols.
If the mother is Rh negative, think if the patient needs an isoimmunization with Anti-D IgG! You have up to 72 hours from the injury to sort it out…
Now, considering the patient was a minor trauma reporting only multiple contusions, it is always better to maintain in-hospital observation for at least 24-48 h. This could be done either in the gynecological or surgical ward, according to hospital policy.
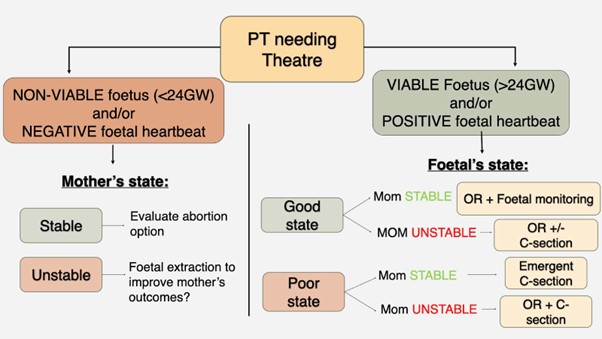
On the other hand, what if the patient needs a surgical intervention? Below there is a flowchart that takes into consideration the mother’s hemodynamic status and the fetal status.
Anexos:
Approximately, only one-third of the radiation dose that the mother receives will arrive at the fetus. So, it is important not to delay images when it’s properly indicated! In these cases, imaging may save lives. So better not to avoid it.
Up to 50 mGy is considered a safe dosage. Consider that a plain chest x-ray is 0.002 mGy and a pelvic x-ray is 0.6 mGy… Those must be done without any doubt.
If the patient needs an abdominal CT scan, it can be done (usually it is up to 35 mGy). On the other hand, if there is a risk of overcoming the 50 mGy limit due to angiography, or multiple or repeated imaging explorations, this possibility should be discussed between the treating team and the patient.
Remember that the patient will have a wider pubic space due to the pregnancy: the symphysis pubis widens up to 4-8 mm.
Gadolinium-based contrast agents may be considered when maternal benefit outweighs potential fetal risks.
| Chest X-Ray | 0.002 mGy |
| Pelvic X-Ray | 0.6 mGy |
| Abdominal CT Scan | 1.3-35 mGy |
| Abdomino-Pelvic CT Scan | 13-25 mGy |
| Angiography | 6.7-56 mGy |
Obstetric Complications Due to Traumatic Causes
- Abruptio Placentae – This should be suspected in every acceleration/deceleration mechanism. Almost 10% of patients with this kinetic, firstly labeled as having “only small contusions”, later developed symptoms from placenta abruption. The clinical scenario may vary from asymptomatic, to massive vagina hemorrhage, to abortion. Treatment is to try to finalize the pregnancy as long as possible and revert the hemorrhagic shock which is often associated with DIC.
- Uterine Rupture – Always correlated to a high energy impact (penetrating>blunt). The major risk factor is a previous uterine scar. It may present with fetal bradycardia, direct palpation of the fetus at the abdominal examination, or intra-abdominal bleeding. Treatment is surgical: laparotomy, fetal extraction, and uterine repair/hysterectomy.
Sometimes things may not go as planned and everything crashes… So, a pregnant lady may suffer a cardiac arrest. Here are a few tips and tricks that may help during a CPR (always hoping you won’t have to use ‘em):
| Action | Reason |
|---|---|
| Increase strength in thoracic compression | Decreased thoracic compliance Diaphragmatic elevation |
| Lateralize uterus to the left / Roll the pt to the left of 15-30° | Decrease compression on the inferior vena cava Increase cardiac pre-load |
| Thoracic compression on top of the sternum | Diaphragmatic elevation |
| IV lines higher than the diaphragm | Aortic-Caval compression |
| Take out fetal monitors before defibrillation | Burn risk |
| The defibrillator pad shifted to the midline | Heart rotation to the right Breast hypertrophy |
| Heimlich maneuver on thorax | Diaphragmatic elevation |
| Emergent C-section after 5 minutes of cardiac arrest | Decrease compression on the inferior vena cava Try to save the baby (if >24 weeks) |
The handover is finished! You have to get back to your patient!!!
The patient is passed on the trauma bed with a 20° left tilt with progressive regain of tension.
A – Open airway, pt alert, the collar on site, central trachea;
B – Hypomobility of the left chest, diminished breath sounds on the left side, bruises on the left side, SatO2 97% on room air, start O2 support with a no-rebreathable mask to increase SatO2 at 100%;
C – 120/75 mmHg, 124 bpm R, belt sign on the belly, pelvis stable on palpation, suspect right femur fracture for deformation and pain on the right thigh, peripheral pulses present, no external bleeding. 500 cc of warm ringer in, ABG, blood test, and blood compatibility tests, right leg on traction;
D – GCS 13 (E3V4M6), pupils equal and reactive to light, no lateralizing signs;
E – Temp 36°C, multiple bruises on the whole body, 5 cm scalp laceration on the left temporal side with no active bleeding;
F – Done by the ObsGyn: Baby with an active heartbeat, slightly bradycardic, apparently no signs of suffering;
E-FAST – Free fluid in the pelvis and the splenorenal space, normal lung sliding on both sides, no hemothorax bilaterally, no pericardial effusion;
Chest X-Ray – Lung contusions on the left side, multiple rib fractures on the left hemithorax;
Pelvic X-Ray – Physiological widening of the pubis, no signs of fractures;
ABG – pH 7.49, pO2 88, pCO2 32, HCO3– 15, Lac 2.2, BE -2, Hb 13
The patient has regained normal blood pressure (125/80 mmHg), the heartbeat is decreasing (110 bpm R), and the GCS is improving as well (GCS 14 – E4V4M6). The ObsGyn colleague starts to be relaxed and happy with the baby’s heartbeat.
The plan now is to study the patient with a CT scan (head, C- spine, and abdomen) and a radiograph of the right femur.
Femur x-ray shows a mid-shaft fracture with good alignment thanks to traction, so the pt is moved to the CT scan next to the trauma bay.
The patient is positioned in the CT scan maintaining the left tilt and the imaging of the head and C-spine is obtained. As soon as the machine stops the patient starts screaming due to heavy uterine contractions.
The patient’s hemodynamic status hasn’t changed, as for physical exploration and E-FAST (still a small amount of fluid in the pelvis and splenorenal space).
What is changing is the tocography which shows a worsening in the baby’s bradycardia. A new ultrasound is done revealing an abruptio placentae!
The team decided to move the patient to the OR for an emergent C-section. The abdominal CT scan may be done afterward if the patient is stable…
Good luck baby!
As always… Hope to see you all very soon!
Namasté…
References
- Advanced Trauma Life Support: Student Course Manual. 10th Ed. Chicago, IL: American College of Surgeons; 2018.
- Lucia A, et al. Trauma Management of the Pregnant Patient. Crit Care Clin 2016;32:109-17.
- Guia clínica per al maneig de la pacient obstétrica amb politraumatisme. CSPT-DC-059 (2018), Hospital Parc Taulí, Sabadell, Barcelona
- Petrone P, et al. Abdominal injuries in pregnancy: a 155-month study at two level 1 trauma centers. Injury 2011;42:47-9.
- Chames MC, et al. Trauma during pregnancy: outcomes and clinical management. Clin Obstet Gynecol 2008;51:398-408.
- Pilkington S, et al. Increase in Mallampati score during pregnancy. Br J Anaesth 1995;74:638-42.
- Richards JR, et al. Blunt abdominal injury in the pregnant patient: Detection with US. Radiology 2004;233:463-70.
- Schiff MA, et al. Pregnancy outcomes following hospitalization for motor vehicle crashes in Washington State from 1989 to 2001. Am J Epidemiol 2005;161:503-10.
- Raja AS, et al. Trauma in pregnancy. Emerg Med Clin North Am 2012;30:937-48.
- Morris JA Jr, et al. Infant survival after cesarean section for trauma. Ann Surg 1996;223:481-8.
- Chibber R, et al. Motor-vehicle injury in pregnancy and subsequent feto-maternal outcomes. J Matern Fetal Neonatal Med 2015;28:399-402.
- Esmaeilzadeh M, et al. One life ends, another begins: management of a brain-dead pregnant mother-a systematic review. BMC Med 2010;8:74.
- Jain V, et al. Guidelines for the management of a pregnant trauma patient. J Obstet Gynaecol Can 2015;37:553-74.
How to Cite This Post
Farré P, Marrano E, Bellio G. Grand Discount – Buy 1, Get 1 for Free. Surgical Pizza. Published on October 31, 2022. Accessed on July 26, 2025. Available at [https://surgicalpizza.org/trauma/grand-discount/].





One Comment
Pingback: